The Downside of Repeat Epidural Steroid Injection Treatments for Lumbar Spinal Stenosis
Published November 16, 2023
Many providers are moving beyond epidural steroid injections (ESIs) for patients with chronic low back pain associated with lumbar spinal stenosis (LSS).
Instead of simply masking the pain caused by an enlarged ligament with epidural injections, which may only provide temporary pain relief, providers now opt for more innovative and durable spinal stenosis treatment options such as the mild® Procedure.
Managing LSS with ESIs
An epidural steroid injection, which is a medication that is injected into the epidural space in the lower spine to reduce swelling and offer pain relief, may be offered to patients with chronic low back pain from conditions such as lumbar spinal stenosis.
Recent data indicates that repeat epidural injections for patients who experience only short-term improvement may not be in the patient’s best interest in the long term. Alternative treatments, such as minimally invasive lumbar decompression, or the mild® Procedure, may be a better option for some patients.
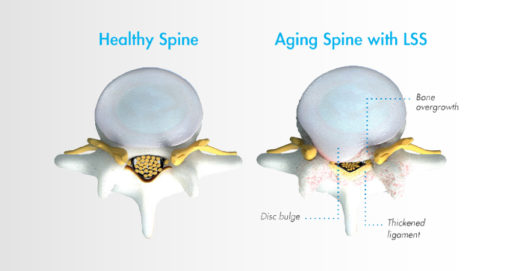
What is LSS?
Lumbar spinal stenosis, also called LSS, contributes to chronic low back pain and is prevalent in approximately 20 percent of patients over the age of 60. LSS is often caused by an enlarged ligament in the back, which compresses the space around the spinal canal and puts pressure on the nerves in the lower back. This pressure around the spinal cord can cause pain, numbness, heaviness, or tingling in the low back, legs, and buttocks. A common visual cue is often referred to as the “shopping cart syndrome,” where the act of leaning over, often over a shopping cart, cane, or walker, helps to temporarily alleviate pressure felt in the lower back pain.
In addition to epidural steroid injections, some common conservative treatment options for LSS can include the mild® Procedure, medication, and/or physical therapy, with more invasive options including procedures such as spacer implants, spinal stenosis surgery, or other open surgery.
How exactly does an ESI work?
Epidural steroid injections are typically offered to LSS patients when more conservative treatment options, such as exercise and physical therapy, have failed to provide relief.
Steroid medication is injected directly into the epidural space, which may relieve pain by reducing inflammation around the spinal cord and nerves. The effects typically last for less than 6 months, after which additional injections may need to be administered.
How effective are ESIs for LSS?
Data shows that epidural steroid injections can effectively relieve pain for LSS patients—but the effects are not lasting, and pain may return, typically in months. ESIs treat the symptoms but do not address the root cause of pain associated with LSS.
The Dark Side of ESIs—The Downsides, Side Effects, and Risks
While ESIs are an effective form of early treatment for some patients, they may not provide reliable, lasting relief for all low back pain.
As mentioned in the Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST), certain payer guidelines, including Centers for Medicare and Medicaid Services (CMS), now stipulate that patients should have obtained a minimum of 3 months of pain relief with eventual recurrence of pain before it is reasonable to proceed with additional injection therapy.
This means that for patients exhibiting shorter-term relief of less than 3 months after receiving an ESI, clinicians should consider alternative treatment options.
ESI treatment may require repeat injections over time
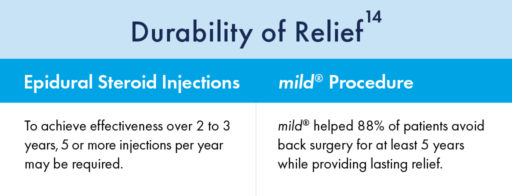
Steroid medication reduces inflammation, which can temporarily relieve pain. However, epidural steroid injections only treat the symptoms of LSS—not the root causes of pain and inflammation. The effects of epidural steroid injections typically last less than 6 months, and patients often require an average of 2–3 injections per year to sustain long-term relief from low back pain associated with LSS.
Repeat ESIs can have negative impacts on patient health
There are many patients for whom repeat epidural steroid injections may offer more risks than benefits. For instance, steroid medications have been linked to bone loss, or osteoporosis. ESIs may also introduce risks for patients with certain comorbidities such as diabetes, cardiovascular conditions, active infections, bleeding disorders, or those taking anticoagulant medications.
As an alternative, epidural injections without the use of steroids may be considered, as well as more advanced decompressive therapies such as the mild® Procedure.
ESI Exhaustion
In addition to the health concerns associated with repeat steroid injections, the mental and emotional effects experienced by many LSS patients can also reveal the dark side of repeat epidural steroid injection treatments.
Due to the temporary nature of epidural steroid injection relief and the requirement for repeat injections, many practices encounter patients with what is increasingly becoming known as “ESI Exhaustion.” ESI Exhaustion can be spotted in patients at any stage of LSS treatment or stenosis severity.
ESI Exhaustion Sign #1: Feelings of Hopelessness
When patients experience short-term relief for a condition as challenging as LSS, they can easily become frustrated and lose hope. LSS patients often experience debilitating pain and loss of mobility that can have a devastating impact on their outlook and optimism for the future. Losing additional time and energy to repeated appointments, procedures, and recovery times can also be detrimental to their quality of life, and some patients may start to feel hopeless if injections remain ineffective or lose their efficacy soon after receiving them.
ESI Exhaustion Sign #2: Decreased Durability of Relief
One of the more common questions patients have about a steroid injection is, “How long will the results last?” Unfortunately, with epidural steroid injections, efficacy can vary by patient, and it can be difficult to predict the degree of relief or durability of effect for the individual. While studies have shown symptom relief for up to 6 months in some lumbar spinal stenosis patients, other studies have demonstrated the limited effectiveness of epidural steroid injections.
ESI Exhaustion Sign #3: Solution Shopping
If patients are dissatisfied with their results and feel they have run out of options in your practice, they may search for another solution. By offering alternative treatments such as the mild® Procedure as an early intervention, you can retain the patients in your practice and increase productivity, while continuing to develop closer relationships and increase your reach within your community.
Avoiding repeat ESIs
Given the significant advances in minimally invasive spine technology, current research confirms that repeat epidural steroid injections should be reserved only for patients who experience significant and lasting relief after the injections, and/or those who are not candidates for higher-level interventions or surgical decompression.
For patients experiencing relief that lasts fewer than 3 months, clinicians may wish to consider more durable treatment options.
Move past injections and make the MOVE2mild®
While they may offer temporary relief, epidural steroid injections do not “cure” LSS. Without addressing the enlarged ligament, which contributes up to 85% of spinal canal narrowing , relief may only be experienced on a short-term or temporary basis.
Minimally invasive lumbar decompression may be the next step for long-lasting relief from LSS and to reduce pressure in the canal. By decreasing the amount of space taken up by the enlarged ligament, patients can experience decreased pressure on the spinal nerves, which may lead to decreased pain.
Performing multiple epidural steroid injections only delays patients from receiving treatment with more lasting results, such as minimally invasive lumbar decompression—the mild® Procedure.
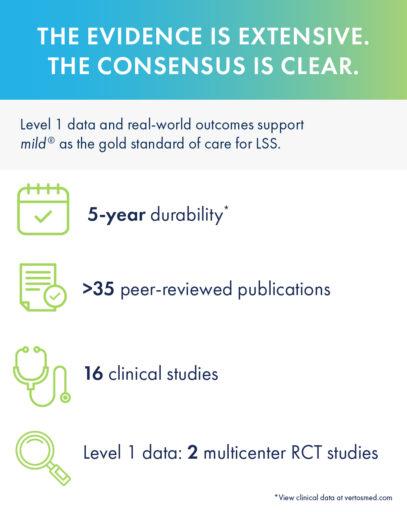
Turning to mild® as the first line of therapy addresses the root cause of LSS by removing excess ligament tissue around the spine, proven to provide a 5-year durability of results.
MOVE2mild® after the first ESI fails
The mild® Procedure is a short, outpatient procedure that can be performed using only local anesthetic and light sedation. The procedure is performed through a single incision in the low back smaller than the size of a baby aspirin, or the diameter of a drinking straw (5.1mm).
By removing excess ligament tissue that has built up around the spine, mild® restores space in the spinal canal. This reduces pressure on the nerves in the low back, addressing a major root cause of LSS, which can help reduce pain.
- The mild® Procedure does not leave an implant behind, and patients typically resume normal activity in 24 hours with no restrictions
- mild® does not require stitches, staples, or complex bandaging
- Typically, patients leave the outpatient procedure facility with just a Band-Aid covering their incision and visit their doctor a few days post-procedure for a quick wound check to ensure healing is progressing normally
- The safety profile of mild® is similar to epidural steroid injections, but with lasting results
- mild® has been shown to provide lasting relief, with 88% of patients avoiding open back surgery for at least 5 years

The mild® Difference
When Epidural Steroid Injections (ESIs) Don’t Provide Lasting Relief, mild® can improve patient outcomes across a variety of measures:
Walking/Standing
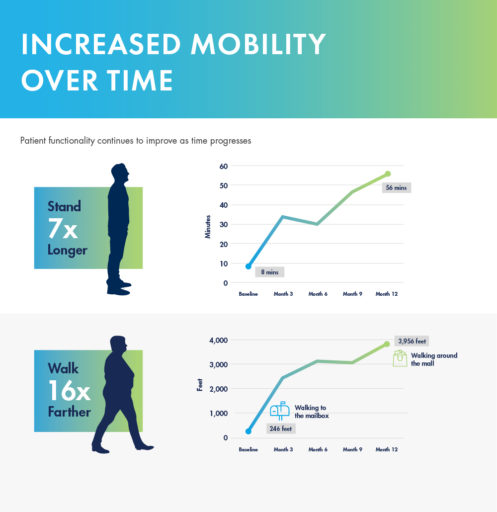
In a study performed at the Cleveland Clinic 1 year after the mild® Procedure, patients were able to:
- increase their standing time from 8 minutes to 56 minutes with less pain.
- increase their average walking distance from 246 feet (comparable to walking to the mailbox) to 3,956 feet (comparable to walking around the mall).
Pain Relief & Mobility
mild® demonstrated excellent long-term durability with significant improvements in both pain and mobility over 2 years. Clinical data from the MiDAS ENCORE 2-Year Study finds mild® provided patients with lasting pain relief and increased mobility.
Long-Term Durability
A 5-year study performed at the Cleveland Clinic demonstrated that mild® helped 88% of patients avoid back surgery for at least 5 years while providing lasting relief. Use our Find a mild® Doctor tool to connect with an interventional pain management specialist in your local area to find out if mild® is right for you.
To learn more about mild® and how it can help people suffering from LSS get on the path to lasting relief, explore mildprocedure.com.