Creating Your mild® Talk Track: 3 Simple Steps APPs Can Take Today to Enhance Patient Education (with Video Demonstration and Helpful Resources)
Author— Ashley Comer, A.P.R.N., NP-C
Advanced Practice Providers (APPs) play a vital role in helping patients understand their lumbar spinal stenosis (LSS) diagnosis and treatment recommendations. By developing strong provider-patient communication, you’re taking the first step towards achieving positive outcomes and enhancing the patient experience.
Why is patient education so important?
- Limited health literacy is linked to a spectrum of suboptimal health outcomes, including increased reports of poor physical functioning, pain, limitations in activities of daily living, and poor mental health status (Source)
- Only about 12 percent of U.S. adults demonstrate proficient health literacy skills (Source)
- Limited health literacy disproportionately affects adults aged 65 and older (Source)
Based on the data above, it is clear that patients over 65 years of age–the group most likely to suffer from LSS–may need more support to understand their condition and treatment plan. With the recognition that both lumbar spinal stenosis and poor health literacy can increase your patients’ susceptibility to poor physical functioning, pain, and limitations in activities of daily living, APPs should feel especially empowered to engage patients. This includes helpful education and dialogue that supports their understanding and helps them feel more comfortable taking the next step on their path to lasting relief.
In the following article, you will find step-by-step guidance and pragmatic suggestions that you can start using today, to help you ensure that your patients leave their consultation feeling confident and excited about their opportunity to make the move to mild®.
Watch: See APP Ashley Comer’s complete talk track for presenting mild® to her LSS patients.
Teach Patients About mild® in 3 Easy Steps
Use the mild® patient brochure as a tool and follow these simple steps to help your patients better understand their lumbar spinal stenosis diagnosis and the benefits of the mild® Procedure.
![]()
Skip the Medical Jargon
Instead of using complex medical terms or acronyms, simplify your explanation with common words, phrases, and analogies to help patients understand their diagnosis and treatment options.
According to the CDC, nearly 9 out of 10 adults struggle to understand and use personal health information when it’s filled with unfamiliar or complex terms. (Source)
On the first page of the mild® patient brochure, you’ll find helpful illustrations that demonstrate the anatomical changes associated with LSS and the symptoms patients typically experience. During your patient consultation, be sure to highlight:
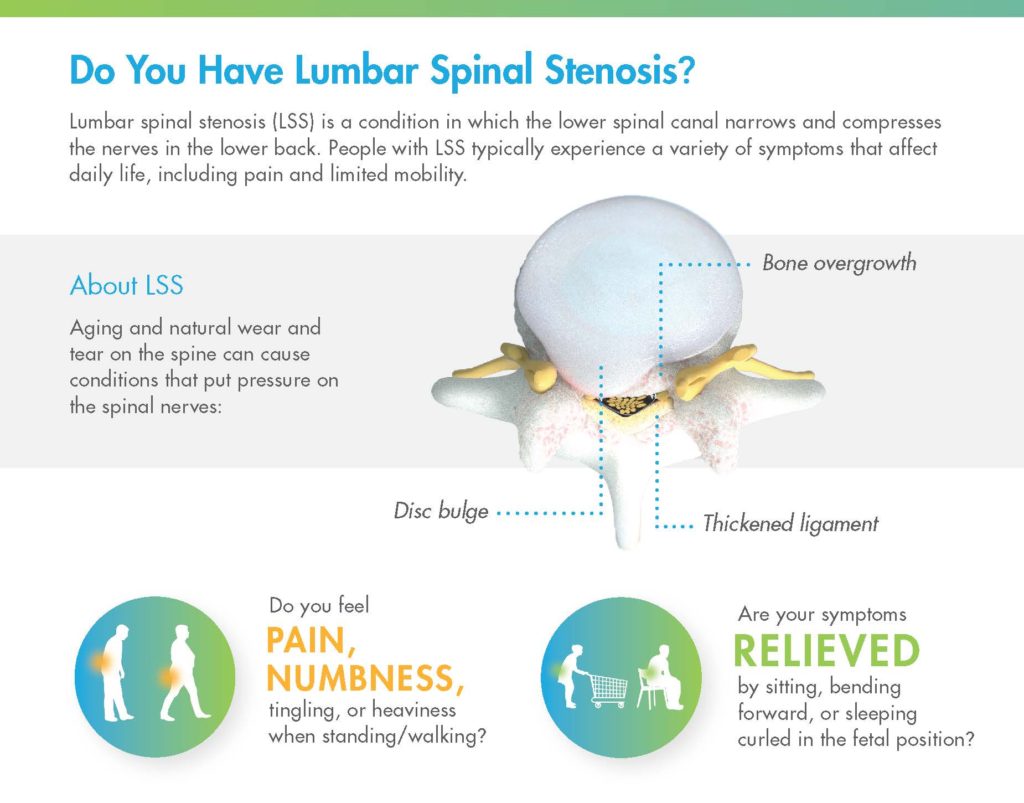
- Compression of the nerves in the lower back.
- LSS can develop as a result of aging and natural wear and tear on the spine
- Thickened ligament is a major root cause of lumbar spinal stenosis
- Symptoms are caused by pressure on spinal nerves
- LSS symptoms affect daily life, causing pain and limited mobility. ASK YOUR PATIENT:
- Do you feel pain, numbness, tingling, or heaviness when standing or walking?
- Are your symptoms relieved by sitting, bending forward, or sleeping in the fetal position?
![]()
Relate LSS to Common, Lived Experiences
Many APPs and physicians use common, real-life analogies to help patients identify and understand their LSS symptoms. A common analogy that many patients may relate to is the “shopping cart syndrome.” Explaining that patients with lumbar spinal stenosis often feel relief when bending over a shopping cart (because it reduces pressure on the compressed nerves) can help patients recognize how this condition impacts their daily life.
STEP 2: Make the Discussion Specific to Your Patient
Once you’ve established the common signs and symptoms of LSS, demonstrate what the MRI shows for that specific patient. Turn to the last page of the mild® patient brochure, where you can use the diagrams provided. Drawing directly on the patient brochure, indicate the following:
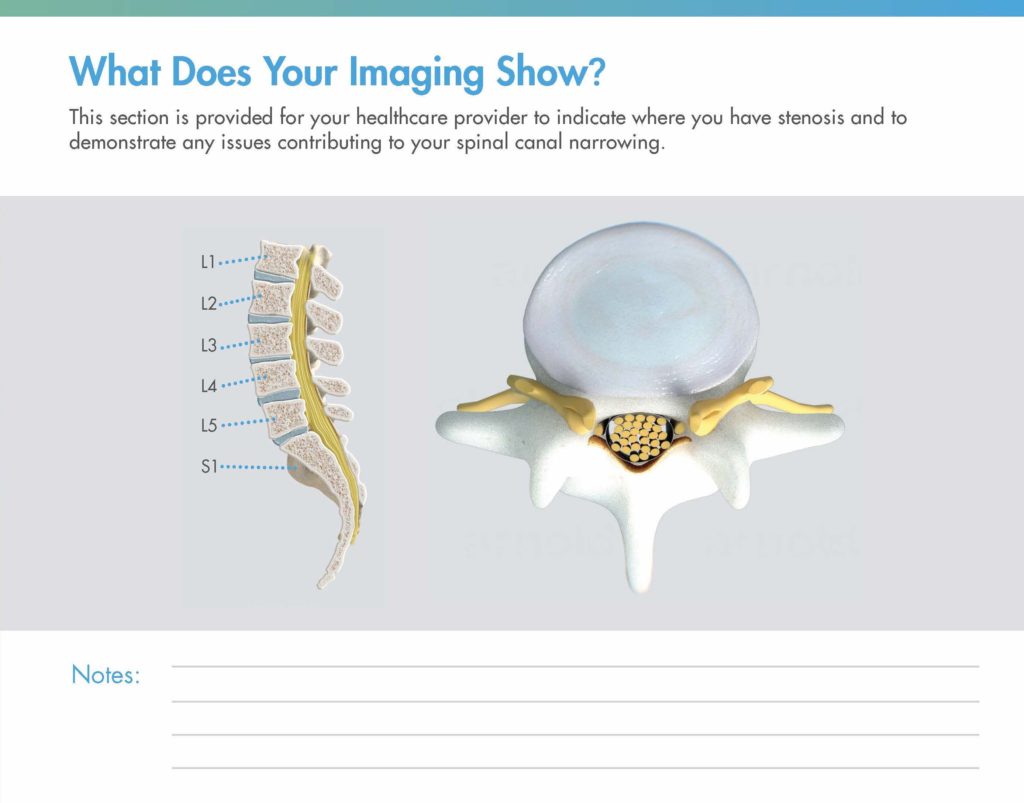
- In the sagittal view on the left, note which level(s) are affected
- In the axial view on the right, show how their thickened ligament appears in the MRI, being sure to draw over the nerves to demonstrate the impact on the central canal
Watch: See how APP Ashley Comer uses the illustrations in the mild® patient brochure to demonstrate her patients’ specific areas of stenosis.
You can also accompany the spinal illustrations in the mild® patient brochure with an added tool, such as a spine model or the patient’s MRI to reinforce the anatomical positioning of the problem or validate the diagnosis, respectively.
STEP 3: Highlight how the mild® Procedure Works
Once patients fully understand their condition, walk them through all of the reasons why you recommend they make the move to mild®. If you turn back to the beginning of the brochure (or access the same information in the mild® patient flip chart) and review the remaining pages, you can quickly cover the advantages of mild® relative to other treatment options, and prepare your patients for what to expect during and after their mild® Procedure.
MOVE2mild®
Because epidural steroid injections (ESIs) were historically the standard of care for lumbar spinal stenosis patients, your patient may be expecting you to recommend another injection. You can explain that the data shows that there is no benefit to giving more than one ESI before mild®, and that giving more than one ESI delays the patient from receiving the longer-lasting, more effective mild® Procedure.
Page 3: How mild® Removes the Problem and Leaves Nothing Behind
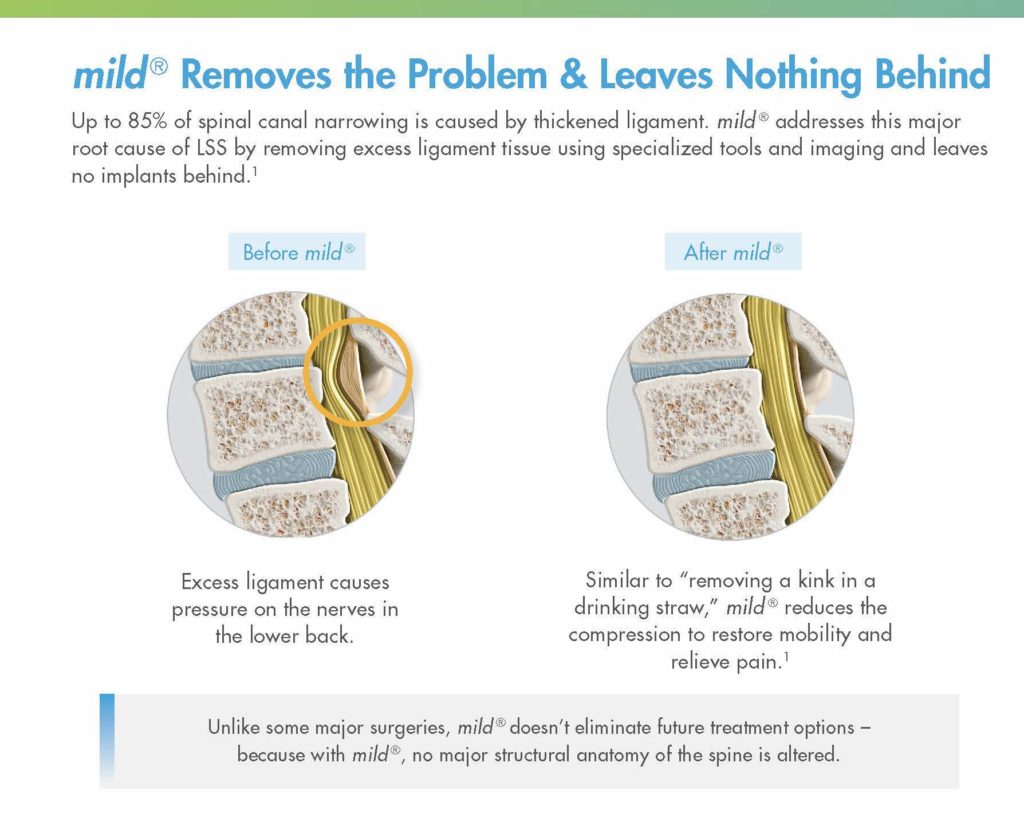
- mild® addresses a major root cause of LSS by removing excess ligament tissue
- mild® reduces compression on the nerves to restore mobility and relieve pain
- mild® doesn’t eliminate future treatment options, as no major structural anatomy of the spine is altered
Page 4: What to Expect on the Day of the mild® Procedure

- Short outpatient procedure
- Can be performed using local anesthetic and light sedation
- Incision smaller than the size of a baby aspirin
- Patients typically resume normal activity within 24 hours with no restrictions
Page 5: What to Expect After the mild® Procedure
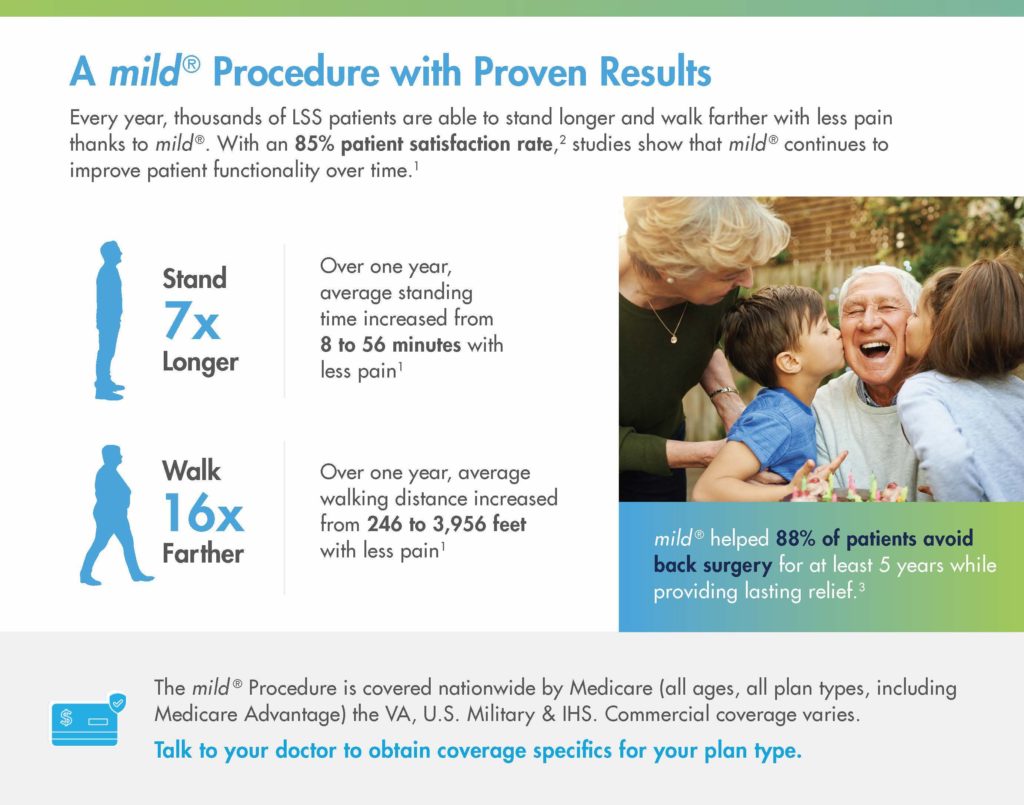
- mild® has an 85% patient satisfaction rate
- mild® continues to improve patient functionality over time
- Over one year, average standing time increased 7x from 8 to 56 minutes with less pain
- Over one year, average walking distance increased 16x from 246 to 3,956 feet with less pain
- mild® helped 88% of patients avoid back surgery for at least 5 years, while providing lasting relief
- mild® is covered nationwide by Medicare and Medicare Advantage. Commercial coverage and other plans vary.
Setting Expectations Supports Patient Success
![]()
Every year, thousands of lumbar spinal stenosis patients are able to stand longer and walk farther with less pain thanks to the mild® Procedure, but those results aren’t achieved overnight. Improvements in patient functionality are typically achieved over time, with patients gradually increasing standing time and walking distance. If you set expectations in advance, patients may be more excited and satisfied to see their own functional improvements over time.
BONUS: Tips to Make Patient Education More Impactful
- Project confidence. When you showcase your knowledge and present information in ways patients can easily understand, they may feel more comfortable making decisions and following your recommendations.
- Encourage patients to ask questions. Take a moment between steps to confirm your patient understands the key points before moving to the next point.
- Discuss the benefits of reconditioning. When setting expectations around recovery, discuss the ways that patients can participate in improving their functionality. Help your patients get back on their feet by suggesting progressively longer walks, or even physical therapy.
Better Patient Education Helps Drive Success with mild®
LSS patients rely on APPs as critical members of their care team. Across the patient journey from diagnosing your patients’ LSS to finding relief with the mild® Procedure, APPs are key in supporting patients, helping them understand their condition, and feeling confident about their decision to make the move to mild®.
At Vertos, we recognize and support the role of APPs and are committed to providing education and resources that help you put more LSS patients on the path to lasting relief.
Don’t miss out on the latest and greatest tips and tools from Vertos.
- Register as an APP to stay informed of new peer-to-peer learning and other educational opportunities
- Follow us on social


- Connect with your Vertos rep for educational resources
Benyamin RM, Staats PS, MiDAS ENCORE Investigators. mild® is an effective treatment for lumbar spinal stenosis with neurogenic claudication: MiDAS ENCORE Randomized Controlled Trial. Pain Physician. 2016;19(4):229-242.
Mekhail N, Costandi S, Abraham B, Samuel SW. Functional and patient-reported outcomes in symptomatic lumbar spinal stenosis following percutaneous decompression. Pain Pract. 2012;12(6):417-425. doi:10.1111/j.1533-2500.2012.00565.x.
2012 data from Health Market Sciences report for Vertos Medical 2013.
Data on file with Vertos Medical.
Staats PS, Chafin TB, Golvac S, et al. Long-term safety and efficacy of minimally invasive lumbar decompression procedure for the treatment of lumbar spinal stenosis with neurogenic claudication: 2-year results of MiDAS ENCORE. Reg Anesth Pain Med. 2018;43:789-794. doi:10.1097/AAP.0000000000000868.
Based on mild® Procedure data collected in all clinical studies. Major complications are defined as dural tear and blood loss requiring transfusion.
MiDAS ENCORE responder data. On file with Vertos Medical.
Jain S, Deer TR, Sayed D, et al. Minimally invasive lumbar decompression: a review of indications, techniques, efficacy and safety. Pain Manag. 2020;10(5). https://doi.org/10.2217/pmt-2020-0037. Accessed June 1, 2020.
Deer TR, Grider JS, Pope JE, et al. The MIST Guidelines: the Lumbar Spinal Stenosis Consensus Group guidelines for minimally invasive spine treatment. Pain Pract. 2019;19(3)250-274. doi:10.1111/papr.12744.
Hansson T, Suzuki N, Hebelka H, Gaulitz A. The narrowing of the lumbar spinal canal during loaded MRI: the effects of the disc and ligamentum flavum. Eur Spine J. 2009;18(5):679-686. doi:10.1007/s00586-009-0919-7.
Treatment options shown are commonly offered once conservative therapies (e.g., physical therapy, pain medications, chiropractic) are not providing adequate relief. This is not intended to be a complete list of all treatments available. Doctors typically recommend treatments based on their safety profile, typically prioritizing low risk/less aggressive procedures before higher risk/more aggressive procedures, but will determine which treatments are appropriate for their patients.
The mild® Procedure is a minimally invasive treatment for lumbar spinal stenosis. As with most surgical procedures, serious adverse events, some of which can be fatal, can occur, including heart attack, cardiac arrest (heart stops beating), stroke, and embolism (blood or fat that migrates to the lungs or heart). Other risks include infection and bleeding, spinal cord and nerve injury that can, in rare instances, cause paralysis. This procedure is not for everyone. Physicians should discuss potential risks with patients. For complete information regarding indications for use, warnings, precautions, and methods of use, please reference the devices’ Instructions for Use.
Patient stories on this website reflect the results experienced by individuals who have undergone the mild® Procedure. Patients are not compensated for their testimonial. The mild® Procedure is intended to treat lumbar spinal stenosis (LSS) caused by ligamentum flavum hypertrophy. Although patients may experience relief from the procedure, individual results may vary. Individuals may have symptoms persist or evolve or other conditions that require ongoing medication or additional treatments. Please consult with your doctor to determine if this procedure is right for you.
Reimbursement, especially coding, is dynamic and changes every year. Laws and regulations involving reimbursement are also complex and change frequently. Providers are responsible for determining medical necessity and reporting the codes that accurately describe the work that is done and the products and procedures that are furnished to patients. For this reason, Vertos Medical strongly recommends that you consult with your payers, your specialty society, or the AMA CPT regarding coding, coverage and payment.
Vertos Medical cannot guarantee coding, coverage, or payment for products or procedures. View our Billing Guide.
Vertos is an equal employment opportunity workplace committed to pursuing and hiring a diverse workforce. We strive to grow our team with highly skilled people who share our culture and values. All qualified applicants will receive consideration for employment without regard to sex, age, color, race, religion, marital status, national origin, ancestry, sexual orientation, gender identity, physical & mental disability, medical condition, genetic information, veteran status, or any other basis protected by federal, state or local law.
Hall S, Bartleson JD, Onofrio BM, Baker HL Jr, Okazaki H, O’Duffy JD. Lumbar spinal stenosis. Clinical features, diagnostic procedures, and results of surgical treatment in 68 patients. Ann Intern Med. 1985;103(2):271-275. doi:10.7326/0003-4819-103-2-271.
Kalichman L, Cole R, Kim DH, et al. Spinal stenosis prevalence & association with symptoms: The Framingham Study. Spine J. 2009;9(7):545-550. doi:10.1016/j.spinee.2009.03.005.
Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998;14(2):148-151. doi:10.1097/00002508-199806000-00010.
Mekhail N, Costandi S, Nageeb G, Ekladios C, Saied O. The durability of minimally invasive lumbar decompression procedure in patients with symptomatic lumbar spinal stenosis: Long-term follow-up [published online ahead of print, 2021 May 4]. Pain Pract. 2021;10.1111/papr.13020. doi:10.1111/papr.13020
Friedly JL, Comstock BA, Turner JA, et al. Long-Term Effects of Repeated Injections of Local Anesthetic With or Without Corticosteroid for Lumbar Spinal Stenosis: A Randomized Trial. Arch Phys Med Rehabil. 2017;98(8):1499-1507.e2. doi:10.1016/j.apmr.2017.02.029
Pope J, Deer TR, Falowski SM. A retrospective, single-center, quantitative analysis of adverse events in patients undergoing spinal stenosis with neurogenic claudication using a novel percutaneous direct lumbar decompression strategy. J Pain Res. 2021;14:1909-1913. doi: 10.2147/JPR.S304997
Pryzbylkowski P, Bux A, Chandwani K, et al. Minimally invasive direct decompression for lumbar spinal stenosis: impact of multiple prior epidural steroid injections [published online ahead of print, 2021 Aug 4]. Pain Manag. 2021;10.2217/pmt-2021-0056. doi:10.2217/pmt-2021-0056
Abstract presented at: American Society of Pain and Neuroscience Annual Conference; July 22-25, 2021; Miami Beach, FL.
Mobility Matters: Low Back Pain in America, Harris Poll Survey, 2022. View data and full summary here.
Deer TR, Grider JS, Pope JE, et al. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. Published 2022 May 5. doi:10.2147/JPR.S355285.